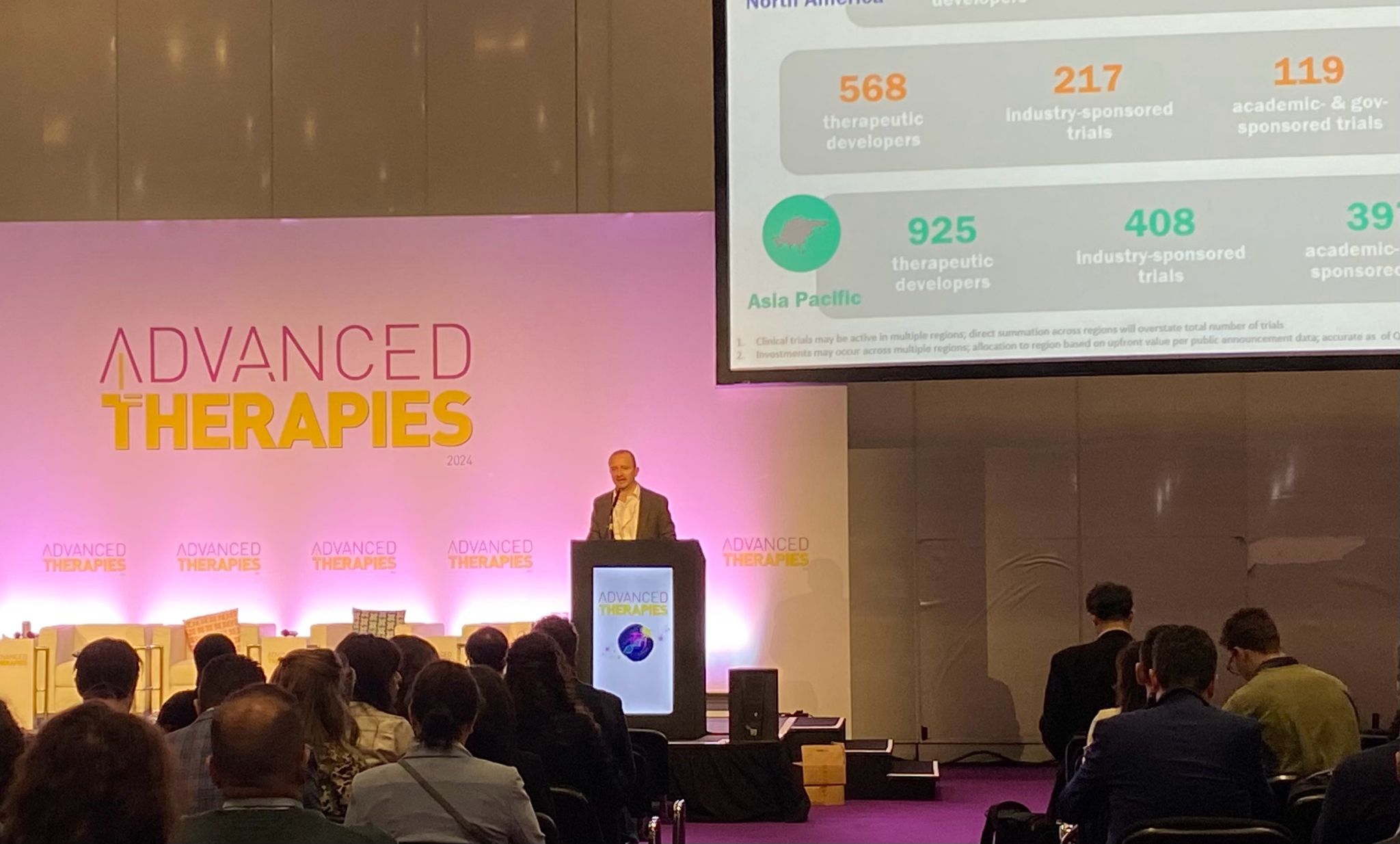
Our Scientific Director, Dr Ann Smith was pleased to attend the 2024 Advanced Therapies Congress at the London ExCeL recently. With over 2000 attendees, and 250 global expert speakers, this event underscores the increasing importance of cellular therapies as a significant component of 21st century medicine. The congress explored the current state of stem cell therapies and focussed on cutting-edge research and new clinical applications. Dr Smith has highlighted the key topics that tapped into recent advances in cord blood stem cell research and treatments.

The congress explored the current state of stem cell therapies and focussed on cutting-edge research and new clinical applications. Dr Smith has highlighted the following key topics that tapped into recent advances in cord blood stem cell research and treatments.
Cord blood and treatment of neurological conditions
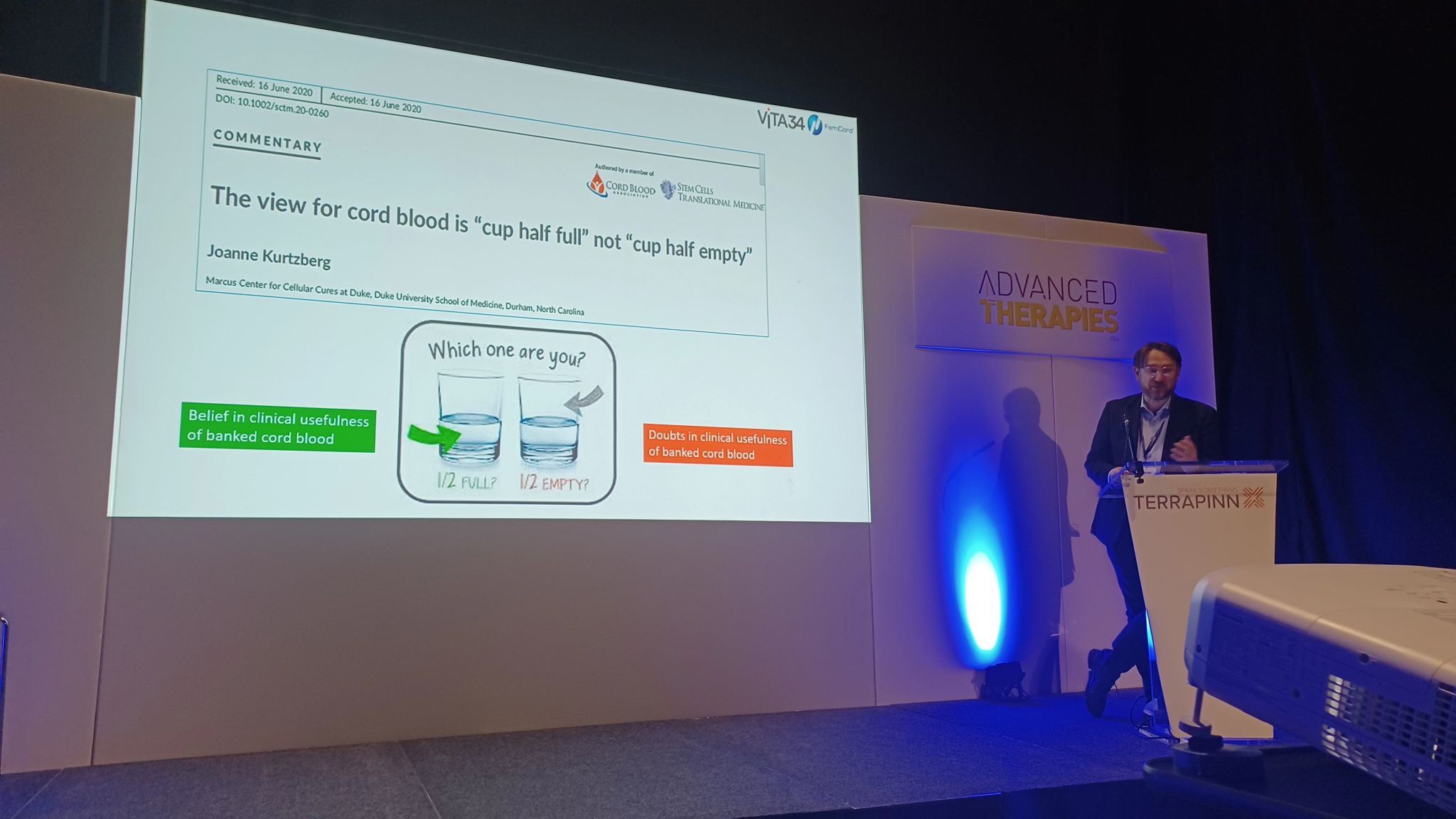
Dr Kurtzberg is a renowned expert in paediatric haematology, cord blood transplantation and novel applications of cord blood stem cells in regenerative medicine at Duke University Hospital, USA and is Director of the Marcus Centre for Cellular Cures (MC3). She gave an update on the current MC3 pipeline of “bench to bedside” trials and innovations.
Dr Kurtzberg highlighted the ground-breaking use of donated cord blood stem cells in the treatment of leukodystrophies which are a group of rare, genetic disorders that affect the white matter of the brain. The condition results in abnormalities or destruction of myelin, a material which covers and protects nerves in the nervous system. The Duke team have identified key cells which are referred to as DUOC-01 cells, within cord blood that are able to help repair damaged myelin. These cells, which are produced from cord blood in the laboratory can be stored in a frozen state ready to treat patients.
Paediatric patients with leukodystrophies are typically treated with donor bone marrow or cord blood transplantation which is designed to slow down the progression of central nervous system damage, but the beneficial effect can take many months to develop and meantime the damage progresses. To address this, DUOC-01 cells are infused intrathecally (via a lumbar puncture into the cerebro-spinal fluid) after the bone marrow or cord blood transplant as a bridging treatment to help with re-myelination and prevent further nerve damage. Dr Kurtzberg reported that results are encouraging with improved outcomes for children receiving the treatment but she indicated that more data will have to be collected including detailed MRI scans of patients pre and post treatment.
Given the therapeutic potency of DUOC-1 cells, Dr Kurtzberg confirmed that they are being utilised in other neurological applications as part of the MC3 innovation pipeline including a trial being undertaken adults with multiple sclerosis.
It is hoped that the safety profile of the treatments continues to be confirmed and that sufficient positive outcome data can be collected to enable FDA licencing of DUOC-1 therapy.
Cord blood expansion to generate different therapeutic products
Expansion of cord blood stem cells ex vivo (in the laboratory) to yield cellular products capable of specific therapeutic actions is an area that is rapidly evolving, and this was a major focus of several presentations at the congress. New pre-clinical and clinical protocols are being developed to harness the amazing proliferative capacity of cord blood stem cells combined with stringent and sophisticated technologies to control their development into cells with enhanced ability to target different diseases.
A presentation from Deverra Therapeutics, a clinical stage biotechnology company located in Seattle, described a novel cord blood cell expansion technology that provides a platform to generate a range of cellular products from donated cord blood. The products include unmodified and modified (engineered) cell types to boost the patient’s blood and immune system to eliminate cancer and virally infected cells. In essence, the laboratory system utilises donor cord blood as a starting material and under carefully controlled conditions, produces specific cellular end products relevant for the treatment of different disorders. For example, immune cells in cord blood called natural killer cells (NK) cells can be generated to target and destroy acute leukaemia. Preclinical work is underway to take this technology a step further so that NK and other immune cells a can be engineered to allow the cancer killing modules on the cells to be customised depending on the particular target cancer.
Early phase clinical trials have involved the use of Deverra’s expanded cellular products in more than 300 treatments across 5 clinical trials in patients with certain leukaemias and also those with COVID-19. The data collected from these trials have indicated that the therapies are safe, and the next step is to look closely at clinical outcomes.
Cord tissue mesenchymal cells in the treatment of Type 1 diabetes
NextCell Pharma, a Swedish company reported details of their developmental work and clinical use of an advanced mesenchymal stem cell (MSC) therapy called ProTrans which is designed to treat autoimmune conditions such a Type 1 Diabetes (T1D). The ProTrans product which is manufactured from the MSC rich Wharton’s jelly inner layer of donor umbilical cord tissue has been used in recent clinical trials which have proved the safety and benefits of the product. This is an amazing step forward in the treatment of T1D which was estimated to afflict approximately 8.4 million people globally in 2021.
So far patients given a single dose of ProTrans show no adverse effects and the treatment results in maintenance of their own insulin production at the level it was at the time of receiving ProTrans. This is attributable to the ability of MSCs to damp down overactive immune activity and also to exert anti-inflammatory and healing effects. Normally, in these patients, insulin production would be expected to reduce as their disease progresses which would cause them to become even more dependent on injected insulin in order to stay well. Remarkably, ProTrans slows down the advancement of the disease therefore reducing the risk of diabetic complications which can be extremely serious and debilitating. Although the product does not reverse T1D or provide a cure, it means that patients require less insulin therapy. The aim is to include more patients in the trial and conduct longer term follow up.
Finally, an interesting panel discussion
A two-way dialogue session between Dr Kurtzberg, her co-presenters and attendees focussed on several topics around innovative uses for cord blood including the use of privately banked units. It is anticipated that it will become feasible for the use of certain novel therapies to be extended to family banked cord blood units as more clinical trial data is collected, analysed and experience in application grows. Cord blood can be stored for decades, therefore it is reassuring to know that in addition to well established uses, the future holds the potential for many novel therapies to become a reality using family banked cord blood.
In summary, it is apparent that we are witnessing active and productive collaboration between scientists and clinicians in taking translational studies from bench to bedside and in so doing, developing and refining transformative cellular therapies.




Rate this article:










